Embarazo adolescente y deficiencia de micronutrientes: Una revisión crítica
DOI:
https://doi.org/10.54167/tch.v18i3.1592Palabras clave:
anemia, adolescentes, embarazo, micronutrientesResumen
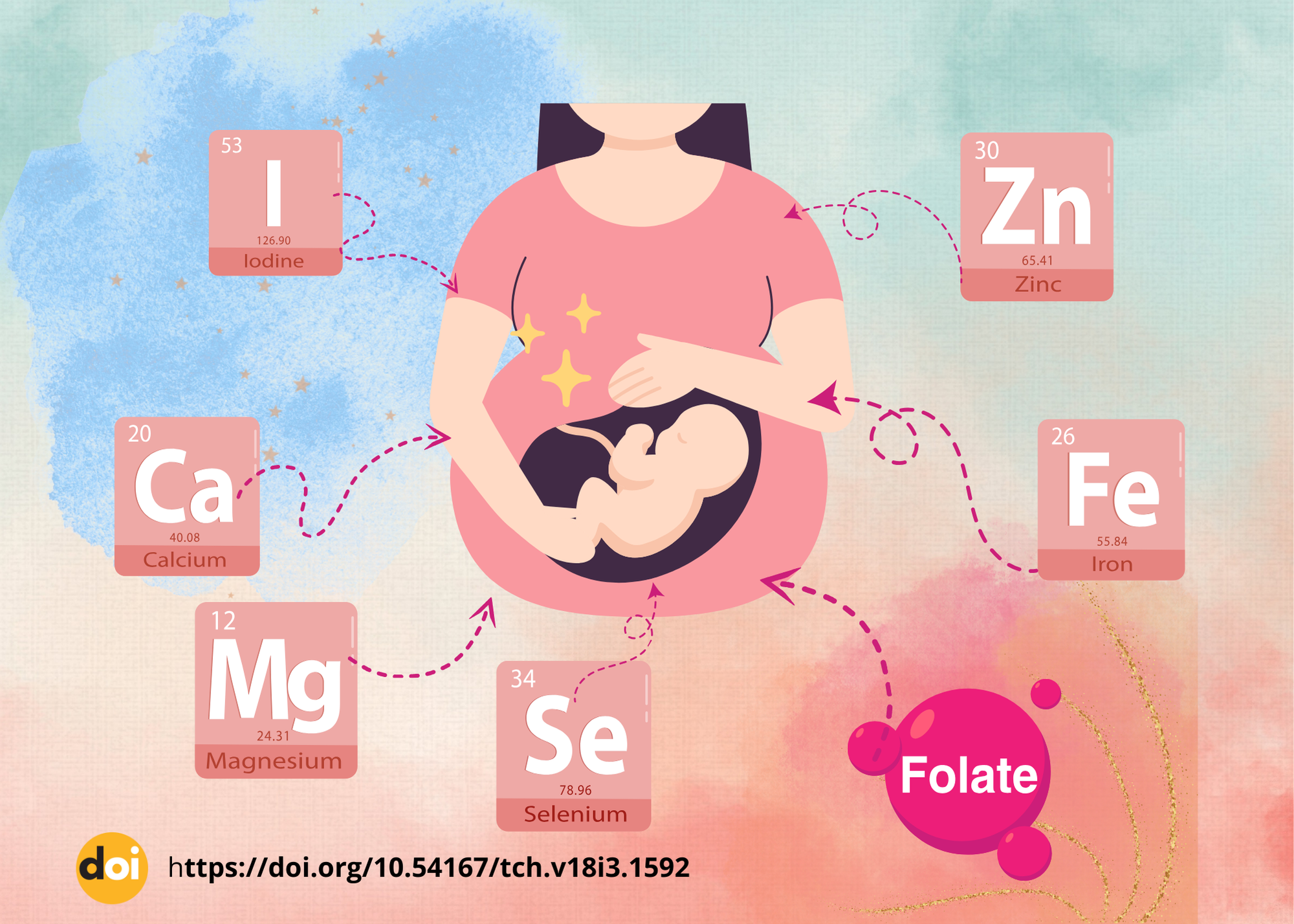
La adolescencia, etapa crítica donde el crecimiento está en su punto máximo y cuando un embarazo ocurre en este período, representa un mayor riesgo nutricional tanto para la madre como para el feto en crecimiento. Las jóvenes adolescentes embarazadas tienen una mayor tendencia de dar a luz a bebés con ciertas anomalías congénitas, menor peso al nacer y mayores posibilidades de mortalidad infantil. La insuficiencia de micronutrientes en la nutrición materna durante la gestación puede aumentar el riesgo de defectos congénitos en los recién nacidos. Esto se puede atribuir a que el feto en desarrollo depende de la nutrición de la madre para su adecuado crecimiento, procesos metabólicos y adecuado desarrollo. La desnutrición durante el embarazo puede provocar una variedad de anomalías congénitas, como defectos de cierre del tubo neural, labio y paladar hendido, defectos cardíacos congénitos y mayor mortalidad fetal. La deficiencia de hierro al inicio del embarazo en el primer y segundo trimestre podría provocar un parto prematuro o una disminución del peso al nacer y un impacto negativo en la salud de los recién nacidos. Pocos de los abortos espontáneos observados en adolescentes durante el primer trimestre podrían atribuirse a la deficiencia nutricional de las madres antes de la concepción.
https://doi.org/10.54167/tch.v18i3.1592
Descargas
Citas
Altura B.M., Li W., Zhang A., Zheng T., Shah N.C., Shah G.J., & Altura B.T. (2016). Sudden Cardiac Death in Infants, Children and Young Adults: Possible Roles of Dietary Magnesium Intake and Generation of PlateletActivating Factor in Coronary Arteries. J. Heart Health 2:(2). http://dx.doi.org/10.16966/2379-769X.121
Amorós R., Murcia M., Ballester F., Broberg K., Iñiguez C., Rebagliato M., Skröder H., González L., Lopez-Espinosa M.-J., & Llop S. (2018). Selenium status during pregnancy: Influential factors and effects on neuropsychological development among Spanish infants. Sci. Total Environ. 610:741–749. https://doi.org/10.1016/j.scitotenv.2017.08.042
Argyridis, S. (2019). Folic acid in pregnancy. Obstet. Gynaecol. Reprod. Med. 29(4): 118–120. https://doi.org/10.1016/j.ogrm.2019.01.008
Babai, A., & Irving, M. (2023). Orofacial Clefts: Genetics of Cleft Lip and Palate. Genes (Basel) 14(8):1603. https://doi.org/10.3390/genes14081603
Bekele, Y., Gallagher, C., Batra, M., Vicendese, D., Buultjens, & M., Erbas, B. (2024). Is Oral Iron and Folate Supplementation during Pregnancy Protective against Low Birth Weight and Preterm Birth in Africa? A Systematic Review and Meta-Analysis. Nutrients 16(16): 2801. https://doi.org/10.3390/nu16162801
Beluska-Turkan, K., Korczak, R., Hartell, B., Moskal, K., Maukonen, J., Alexander, D.E., Salem, N., Harkness, L., Ayad, W., Szaro, J., Zhang, K., & Siriwardhana, N. (2019). Nutritional Gaps and Supplementation in the First 1000 Days. Nutrients 11(12): 2891. https://doi.org/10.3390/nu11122891
Bromage S., Ahmed T., & Fawzi W.W. (2016). Calcium Deficiency in Bangladesh: Burden and Proposed Solutions for the First 1000 Days. Food Nutr. Bull 37(4): 475–493. https://doi.org/10.1177/0379572116652748
Conlon, M.A., & Bird, A.R. (2014). The impact of diet andlifestyle on gut microbiota and human health. Nutrients 7(1):17–44. https://doi.org/10.3390/nu7010017
Cheng, Z., Gu, R., Lian, Z., Gu, H.F. (2022). Evaluation of the association between maternal folic acid supplementation and the risk of congenital heart disease: a systematic review and meta-analysis. Nutr J. Mar 21(1):20. https://doi.org/10.1186/s12937-022-00772-2
Chikakuda, A.T., Shin, D., Comstock, S.S., Song, S., & Song, W.O. (2018). Compliance to prenatal iron and folic acid supplement use in relation to low birth weight in Lilongwe, Malawi. Nutrients 10(9): 1275. https://doi.org/10.3390/nu10091275
de Araújo, C.A.L., Ray, J.G., Figueiroa, J.N., & Alves, J.G. (2020). BRAzil magnesium (BRAMAG) trial: A double- masked randomized clinical trial of oral magnesium supplementation in pregnancy. BMC Pregnancy Childbirth.20:234. https://doi.org/10.1186/s12884-020-02935-7
Elbaz, F., Zahra, S., & Hanafy, H. (2017). Magnesium, zinc and copper estimation in children with attention deficit hyperactivity disorder (ADHD) Egypt J. Med. Hum. Gen. 18(2):153–163. https://doi.org/10.1016/j.ejmhg.2016.04.009
Farías, P.M., Marcelino, G., Santana, L.F., de Almeida, E.B., Guimarães, R.C.A., Pott, A., Hiane, P.A., & Freitas, K.C. (2020). Minerals in Pregnancy and Their Impact on Child Growth and Development. Molecules 25(23): 5630. https://doi.org/10.3390/molecules25235630
Galetti, V., Mitchikpè, C.E.S., Kujinga, P., Tossou, F., Hounhouigan, D.J., Zimmermann, M.B., & Moretti, D. (2016). Rural Beninese children are at risk of zinc deficiency according to stunting prevalence and plasma zinc concentration but not dietary zinc intakes. J. Nutr. 146(1): 114–123. https://doi.org/10.3945/jn.115.216606
Georgieff, M.K. (2020). Iron deficiency in pregnancy. Am. J. Obstet. Gynecol. 223(4): 516-524. https://doi.org/10.1016/j.ajog.2020.03.006
Guo, Y., Zhang, N., Zhang, D., Ren, Q., Ganz, T., Liu, S., & Nemeth, E. (2019). Iron homeostasis in pregnancy and spontaneous abortion. Am. J. Hematol. 94(2): 184–188. https://doi.org/10.1002/ajh.25341
Harvey, L., & Boksa, P. (2014). Additive effects of maternal iron deficiency and prenatal immune activation on adult behaviors in rat offspring. Brain, Behavior, and Immunity 40: 27–37. https://doi.org/10.1016/j.bbi.2014.06.005
Hofstee, P., McKeating, D.R., Bartho, L.A., Anderson, S.T., Perkins, A.V., & Cuffe, J.S. (2020). Maternal selenium deficiency in mice alters offspring glucose metabolism and thyroid status in a sexually dimorphic manner. Nutrients 12(1): 267. https://doi.org/10.3390/nu12010267
Jiang, S., Yang, B., Xu, J., Liu, Z., Yan, C., Zhang, J., Li, S., & Shen, X. (2019) Associations of Internal-Migration Status with Maternal Exposure to Stress, Lead, and Selenium Deficiency Among Pregnant Women in Shanghai, China. Biol. Trace Elem. Res. 190(2): 309–317. https://doi.org/10.1007/s12011-018-1570-0
Jouanne, M., Oddoux, S., Noël, A., & Voisin-Chiret, A.S. (2021). Nutrient Requirements during Pregnancy and Lactation. Nutrients 13 (2): 692. https://doi.org/10.3390/nu13020692
Keats, E.C., Akseer, N., Thurairajah, P., Cousens, S., Bhutta, Z.A., & Global Young Women’s Nutrition Investigators’ Group. (2022). Multiple-micronutrient supplementation in pregnant adolescents in low- and middle-income countries: a systematic review and a meta-analysis of individual participant data. Nutr Rev. 80(2): 141-156. https://doi.org/10.1093/nutrit/nuab004
Mao, J., Vanderlelie, J.J., Perkins, A.V., Redman, C.W., Ahmadi, K.R., & Rayman, M.P. (2016). Genetic polymorphisms that affect selenium status and response to selenium supplementation in United Kingdom pregnant women. Am. J. Clin. Nutr. 103(1): 100–106. https://doi.org/10.3945/ajcn.115.114231
Mosha, D., Liu, E., Hertzmark, E., Chan, G., Sudfeld, C., Masanja, H., & Fawzi, W. (2017). Dietary iron and calcium intakes during pregnancy are associated with lower risk of prematurity, stillbirth and neonatal mortality among women in Tanzania. Public Health Nutr. 20(4): 678–686. https://doi.org/10.1017/s1368980016002809
Nogales, F., Ojeda, M.L., Del Valle, P.M., Serrano, A., Murillo, M.L., & Carreras-Sánchez, O. (2017). Metabolic syndrome and selenium during gestation and lactation. Eur. J. Nutr. 56(2): 819–830. https://doi.org/10.1007/s00394-015-1129-1
Olivo-Vidal, Z.E., Rodríguez, R.C., & Arroyo-Helguera, O. (2016) Iodine affects differentiation and migration process in trophoblastic cells. Biol. Trace Elem. Res. 169(2): 180–188. https://doi.org/10.1007/s12011-015-0433-1
Palacios, C., Kostiuk, L.K., & Peña‐Rosas, J.P. (2019). Vitamin D supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 7(7): CD008873. https://doi.org/10.1002/14651858.cd008873.pub4
Rajwar, E., Parsekar, S.S., & Venkatesh, B.T (2020). Effect of vitamin A, calcium and vitamin D fortification and supplementation on nutritional status of women: an overview of systematic reviews. Syst. Rev. 9: 248. https://doi.org/10.1186/s13643-020-01501-8
Rees, W.D., Hay, S.M., Hayes, H.E., Stevens, V.J., Gambling, L., & McArdle, H.J (2020). Iron deficiency during pregnancy and lactation modifies the fatty acid composition of the brain of neonatal rats. J. Dev. Origins Health Dis. 11(3): 264–272. https://doi.org/10.1017/s2040174419000552
Saydam, B.K., Genc, R.E., Sarac, F., & Turfan, E.C. (2017). Prevalence of anemia and related factors among women in Turkey. Pak. J. Med. Sci. 33(2): 433-438. https://doi.org/10.12669/pjms.332.11771
Shinde, S., Wang, D., Yussuf, M.H., Mwanyika-Sando, M., Aboud, S., & Fawzi, W.W. (2022). Micronutrient Supplementation for Pregnant and Lactating Women to Improve Maternal and Infant Nutritional Status in Low-and Middle-Income Countries: Protocol for a Systematic Review and Meta-analysis. JMIR Res Protoc. 11(8): e40134. https://doi.org/10.2196/40134
Shahid, M.A., Ashraf, M.A., & Sharma, S. (2024). Physiology, Thyroid Hormone. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK500006/
Stoffaneller, R., & Morse, N.L. (2015). A review of dietary selenium intake and selenium status in Europe and the Middle East. Nutrients. 7(3): 1494–1537. https://doi.org/10.3390/nu7031494
Viktorinova, A., Ursinyova, M., Trebaticka, J., Uhnakova, I., Durackova, Z., & Masanova, V. (2016). Changed plasma levels of zinc and copper to zinc ratio and their possible associations with parent-and teacher-rated symptoms in children with attention-deficit hyperactivity disorder. Biol. Trace Elem. Res. 169(1): 1–7. https://doi.org/10.1007/s12011-015-0395-3
Volpe, J.J. (2019). Iron and zinc: Nutrients with potential for neurorestoration in premature infants with cerebral white matter injury. J. Neonatal. Perinatal. Med. 12(4): 365–368. https://doi.org/10.3233/npm-190369
Weaver, C.M., & Heaney, R.P. (2014). Calcium. In: Ross, A.C., Caballero, B., Cousins, R.J., Tucker, K.L., & Ziegler, T.R., editors. Modern Nutrition in Health Disease. 11th ed. Lippincott Williams & Wilkins; Baltimore, MD, USA: 2014. pp. 133–149.
WHO (2016) Recommendations on Antenatal Care for a Positive Pregnancy Experience; World Health Organization: Geneva, Switzerland, 2016. https://iris.who.int/bitstream/handle/10665/259947/WHO-RHR-18.02-eng.pdf
WHO (2017). Nutritional Anaemias: Tools for Effective Prevention and Control. World Health Organization; Geneva, Switzerland https://apps.who.int/iris/bitstream/handle/10665/259425/9789241513067-eng.pdf
WHO (2018). Weekly Iron and Folic Acid Supplementation as an Anaemia-Prevention Strategy in Women and Adolescent Girls: Lessons Learnt from Implementation of Programmes Among Non-Pregnant Women of Reproductive Age. World Health Organization; Geneva, Switzerland. https://apps.who.int/iris/bitstream/handle/10665/274581/WHO-NMH-NHD-18.8-eng.pdf
Wilson, R.L., Bianco-Miotto, T., Leemaqz, S.Y., Grzeskowiak, L.E., Dekker, G.A., & Roberts, C.T. (2018). Early pregnancy maternal trace mineral status and the association with adverse pregnancy outcome in a cohort of Australian women. J. Trace Elem. Med. Biol. 46: 103–109. https://doi.org/10.1016/j.jtemb.2017.11.016
Yimer, B., & Wolde, A. (2022). Prevalence and predictors of malnutrition during adolescent pregnancy in southern Ethiopia: a community-based study. BMC Pregnancy Childbirth 22(1): 130. https://doi.org/10.1186/s12884-022-04460-1
Zimmermann, M.B. (2016). The Importance of Adequate Iodine during Pregnancy and Infancy. World Rev. Nutr. Diet. 115:118–124. https://doi.org/10.1159/000442078
Zemrani, B., & Bines, J.E. (2020). Recent insights into trace element deficiencies: Causes, recognition and correction. Curr. Opin. Gastroenterol 36(2): 110–117. https://doi.org/10.1097/mog.0000000000000612
Zhou, S.J., Condo, D., Ryan, P., Skeaff, S.A., Howell, S., Anderson, P.J., McPhee, A.J., & Makrides, M. (2019). Association between maternal iodine intake in pregnancy and childhood neurodevelopment at age 18 months. Am. J. Epidemiol. 188(2): 332–338. https://doi.org/10.1093/aje/kwy225
Publicado
Cómo citar
-
Resumen120
-
PDF75
-
HTML11
Número
Sección
Licencia
Derechos de autor 2024 TECNOCIENCIA Chihuahua

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.